Breathlessness, common for people with heart and lung conditions, certain cancers, and anxiety, can be debilitating, frightening and distressing for both the sufferer and their loved ones.
At Hospice West Auckland, physiotherapist Marion specialises in respiratory care for patients with breathlessness. As well as providing all aspects of physiotherapy and respiratory care individually to patients and whānau, she runs Puna Haoura Breathe Easy classes for groups at Hospice House every week.
Marion trained as a physiotherapist in her native South Africa. She discovered she loved working in the community, where she had the opportunity to work with other providers such as speech therapists and occupational therapists in a truly multi-disciplinary approach. “It was a chance to give in a different way, not just with physio but with many different skills,” she says. Her next role was split between hospital and musculoskeletal outpatients, which she enjoyed in equal measures. Over the next few years she undertook study in two specialisation fields: sport and cardio respiratory care. Although quite different, both fields were her passion, and she was fortunate to be able to practice in both fields working in a physio clinic.
Marion emigrated to New Zealand several years ago, where she opened her own physio clinic – which she continues to run four days per week. “But I found that I missed the respiratory side and I didn’t want to lose those skills I had gained, so when the position came up at Hospice West Auckland I decided that I needed to do it,” she explains. “I started working at Hospice in 2020, one day per week, and I’ve never looked back.”
The Hospice West Auckland physiotherapists are a multi-skilled team and receive patient referrals via the Hospice nurses. Each therapist provides all aspects of physiotherapy to patients but also specialise in specific areas – such as Marion’s speciality of respiratory care. “When a patient is referred to us, we assess them as a team and determine which of us is best to take the lead in their care,” she explains. “I think our service is very special. We’ve got a really strong model and we’re fortunate to have a team of physiotherapists and all the different specialities.”
“I enjoy the team and the multidisciplinary aspect of our work, going out into the community and seeing patients in their own homes,” says Marion. “When you go out into their homes, you can see what they really need. For example, how far they have to mobilize to the bathroom, and if they need a walking frame are they restricted by a confined space? So we can really tailor our support to every patient.” During home visits, Marion identifies which tools and information for managing breathlessness are most relevant to the person, and teaches both them and their family members. “Family members play a big role in managing breathlessness, which is why I prefer them to be there, both at home visits and the group sessions,” she says. “The family member reinforces the techniques I give, before their loved one becomes too breathless. Once a person becomes breathless they do not think clearly and forget the tools I have taught them. It also gives carers confidence, because it can be very scary watching a loved one struggle to breathe.”
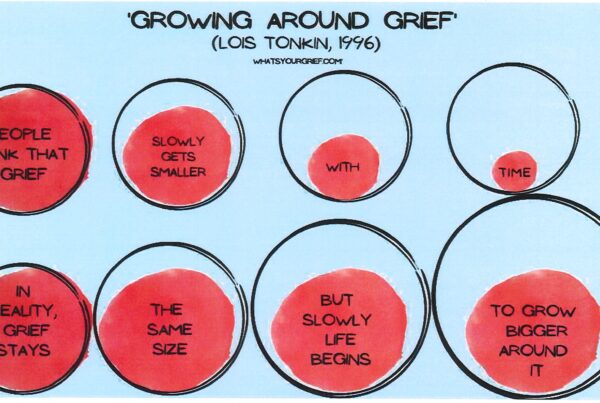
The weekly Puna Haoura Breathe Easy classes Marion runs offer a different dynamic to home visits. The classes have a valuable social element, where you can talk to other patients suffering from breathlessness and share advice and feelings. The sessions are very gentle, based on advice and information with techniques the attendees can take home. “I always compare it to a toolbox,” explains Marion. “I teach them all of the techniques, and they try them and pick the ones that work best for them. I also explain why gentle daily exercise and activities are so important to maintain muscle strength and functionality. It’s easy to become fearful of exercise when you are suffering from breathlessness, but once you have the tools to manage it you can understand that a little bit of breathlessness is fine and be more confident in being active.”

The Breathe Easy ‘Breathing Thinking Functioning’ (BTF) model was developed by the Cambridge Breathlessness Intervention Service. Marion has organised and structured the programme into three weekly sessions that allow attendees to follow on even if they have missed the previous session. “It’s important to maintain flexibility here at Hospice. Sometimes coming to class just isn’t possible, and although attending all three sessions in order is ideal, we need to ensure the classes still work for people who need to drop in and out.” It’s also important that the person’s symptoms and timing are just right to benefit from the tools taught. Patients who are breathless at rest or on exertion, with or without a component of anxiety and deconditioning, and functionally able to attend the group, will benefit most.
Echoing the sentiments of so many who work in Hospice care, Marion emphasises the enjoyment she finds in watching the positive impact she has on patients and whānau, along with the meaningful connections she makes with them. “It can be a juggle to manage my time between my own practice and Hospice, but I always come back to: Hospice gives me joy. I see the difference my advice and teachings give people, and how much it helps them. It’s my feel-good job – it fills my cup.”